Home mechanical ventilation (HMV) encompasses a spectrum of ventilatory support strategies intended for use outside of acute hospital settings, including in patients’ homes, long-term care facilities, or assisted living centers. The choice of ventilation type depends critically on the patient’s underlying condition, tolerance, disease severity, and the availability of caregivers and technical infrastructure.
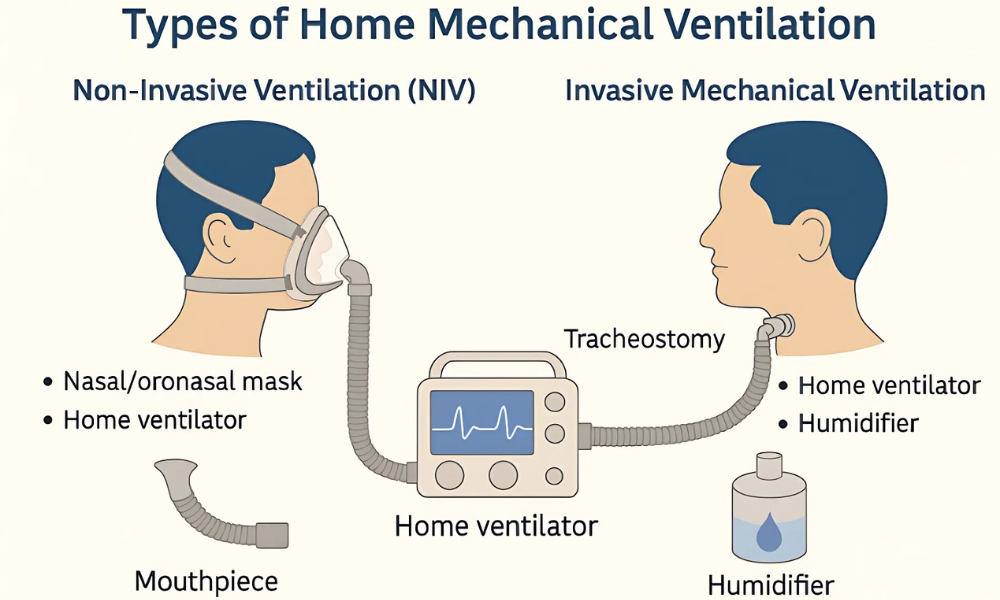
Broadly, HMV can be classified into non-invasive ventilation (NIV) and invasive mechanical ventilation (IMV), each with its own distinct clinical rationale, mode of delivery, and associated outcomes.
Technological advancements have made both modalities increasingly feasible in domiciliary environments. Fagondes et al. (2025) emphasized that the successful adaptation of hospital-grade ventilatory care to home settings has significantly reduced hospitalizations and improved quality of life in patients with chronic respiratory failure (1).
The classification of HMV typically includes:
- Non-Invasive Ventilation (NIV): Delivered via a mask or nasal prongs without requiring tracheal intubation.
- Invasive Mechanical Ventilation (IMV): Delivered via a tracheostomy or endotracheal tube, providing direct access to the airway.
- Hybrid and Specialized Ventilation Techniques: This category includes advanced modes or combinations of ventilation tailored to specific patient needs (e.g., negative pressure ventilation in historical contexts or diaphragm pacing).
- Home Ventilator Equipment and Technology: Encompasses the devices, accessories, and digital solutions (e.g., telemonitoring) that support HMV delivery.
Each approach comes with specific indications, risks, and technological requirements, and is ultimately chosen based on the patient’s clinical and functional profile.
Non-Invasive Ventilation (NIV)
Non-invasive ventilation (NIV) is the most widely adopted modality in home mechanical ventilation (HMV), particularly among adults with chronic obstructive pulmonary disease (COPD), obesity hypoventilation syndrome (OHS), and neuromuscular diseases (NMDs) that involve preserved bulbar function.
NIV delivers ventilatory support via an external interface, such as a nasal mask, oronasal mask, or mouthpiece. This approach cleverly bypasses the need for tracheostomy and its associated risks, including infection and tracheal injury. NIV is frequently initiated during hospitalization and continued at home following patient stabilization (3).
Common ventilation modes in NIV include Continuous Positive Airway Pressure (CPAP), Bilevel Positive Airway Pressure (BiPAP), and hybrid forms like Average Volume-Assured Pressure Support (AVAPS) and intelligent Volume-Assured Pressure Support (iVAPS). These advanced modes can be precisely tailored to patient-specific needs, which is especially crucial in progressive diseases such as Amyotrophic Lateral Sclerosis (ALS) where ventilatory demand fluctuates over time. Modern NIV devices are compact, battery-powered, and often equipped with integrated humidification and telemonitoring capabilities (8).
Studies highlight the clinical benefits of NIV. Ong et al. (2025) reported that integrating transcutaneous CO₂ monitoring into home NIV services significantly improved adherence and therapy titration (5). Scheller (2025) further demonstrated improved survival and reduced hospitalizations in pediatric patients receiving nocturnal NIV (2). For daytime support, mouthpiece ventilation (MPV) is increasingly utilized in high-functioning ALS patients, as it allows for uninterrupted speech and social engagement (11).
| Category | Details |
| Indications | * COPD with chronic hypercapnia * Obesity hypoventilation syndrome (OHS) * Neuromuscular disorders with preserved bulbar function (e.g., ALS, SMA) * Restrictive thoracic diseases (e.g., kyphoscoliosis) |
| Modes | * CPAP – Fixed pressure, mainly for sleep apnea/OHS * BiPAP – Separate inspiratory/expiratory pressures * AVAPS/iVAPS – Adjusts support to achieve a set tidal volume * S/T Mode – Adds a backup respiratory rate in case of apnea |
| Interfaces | * Nasal mask * Oronasal/full-face mask * Mouthpiece (MPV) |
Invasive Mechanical Ventilation (IMV)
Invasive mechanical ventilation (IMV) is delivered via a tracheostomy tube and is considered when non-invasive ventilation (NIV) fails or is inappropriate. This applies to patients with severe bulbar dysfunction, central hypoventilation syndromes (e.g., Congenital Central Hypoventilation Syndrome [CCHS]), or progressive neuromuscular conditions associated with a high aspiration risk (3). While IMV ensures more reliable airway access and enhanced secretion clearance, it inherently introduces higher complexity and a greater risk of complications.
Patients receiving IMV require comprehensive support, which includes dedicated ventilators, humidifiers, suction devices, continuous monitoring, and often 24/7 caregiving. These extensive needs present significant emotional, logistical, and financial challenges for families. However, outcomes can be favorable when supported by a well-structured care model. Wei et al. (2025) documented improved home transition success rates when structured caregiver training and robust safety plans were implemented (9).
Furthermore, Enzer et al. (2025) emphasized the importance of consistent social and institutional support in ensuring long-term IMV success in children (10). Pediatric studies have consistently confirmed that tracheostomy-dependent children can achieve improved stability and reduced hospitalization rates when supported by multidisciplinary teams (4).
| Category | Details |
| Indications | * Amyotrophic Lateral Sclerosis (ALS) with bulbar involvement * Central hypoventilation syndromes (e.g., CCHS) * Severe restrictive thoracic diseases * Chronic hypercapnic respiratory failure unresponsive to NIV |
| Requirements | * Tracheostomy care and suctioning * Continuous pulse oximetry and capnography monitoring * Backup ventilator and battery power * Constant caregiver or nursing presence * Supplemental oxygen or feeding tubes in select cases |
Hybrid & Specialized Ventilation Modes
Some patients benefit from hybrid ventilation strategies where both non-invasive ventilation (NIV) and invasive mechanical ventilation (IMV) are employed in a circadian or disease-stage-dependent pattern. For instance, nocturnal NIV can be used alongside daytime IMV. This approach is particularly relevant in pediatric neuromuscular conditions or during transitions from partial to full ventilatory dependence (3).
Advanced ventilator technologies are increasingly being integrated into HMV. Neurally Adjusted Ventilatory Assist (NAVA), for example, detects diaphragm electrical signals (EAdi) to precisely tailor pressure delivery to patient effort. This mode has shown significant promise in improving synchrony and enhancing extubation success in neonates, and its potential for long-term home use is currently under consideration (12). Similarly, volume-assured modes like iVAPS and AVAPS automatically adjust pressures to maintain set ventilation targets, proving highly beneficial in patients with irregular breathing patterns or progressive disease.
Mouthpiece ventilation (MPV) remains an essential option for patients who require intermittent support during wakeful hours. This method uniquely preserves the ability to speak, eat, and interact—critical factors for maintaining autonomy and quality of life in conditions such as Amyotrophic Lateral Sclerosis (ALS) and other high-functioning neuromuscular disorders (NMDs) (11).
- Hybrid NIV+IMV: Combines non-invasive and invasive support based on time of day or disease progression.
- NAVA: Improves patient-ventilator synchrony and comfort by sensing diaphragm activity.
- iVAPS and AVAPS: Automatically adjust ventilator support to meet changing patient demands and maintain ventilation targets.
- MPV: Enhances autonomy and communication for awake patients requiring intermittent support.
Ventilator Technology and Equipment
The rise of compact and intelligent ventilators has profoundly revolutionized home mechanical ventilation (HMV). Modern devices, offer a comprehensive range of ventilatory modes (including both pressure- and volume-controlled), enhanced portability, and continuous monitoring capabilities. These advancements translate into quieter operation, improved energy efficiency, and a design suited for long-term use, spanning months to years (1).
Key technological enhancements include real-time alarms for critical events like apnea, circuit disconnection, and excessive leaks. Furthermore, these devices often feature programmable day/night cycles for optimized therapy and are fully compatible with essential oxygen and humidification systems. The integration of telehealth functionalities is a significant step forward, enabling clinicians to remotely adjust ventilator settings, download vital adherence data, and proactively intervene in cases of patient deterioration (5).
Despite these substantial advantages, equitable access to modern ventilators and integrated telemonitoring tools remains a significant challenge, particularly in low-resource regions. To ensure safe and truly global HMV deployment, there is a pressing need for the development of simpler, more ruggedized devices, alongside sustained investment in comprehensive caregiver training programs (8).
Key Features of Modern Home Ventilators:
- Customizable Modes: Offers diverse pressure- and volume-controlled ventilation modes for personalized therapy.
- Integrated Safety: Features built-in real-time alarms and robust safety systems (e.g., for apnea, disconnection, leaks).
- Data Connectivity: Enables comprehensive data logging and wireless connectivity for remote monitoring.
- Telehealth Capabilities: Supports remote setting adjustments by clinicians and early intervention based on downloaded adherence data.
- System Compatibility: Designed for seamless integration with humidifiers, supplemental oxygen, and other essential accessories.
| Feature | Non-Invasive Ventilation (NIV) | Invasive Mechanical Ventilation (IMV) |
| Interface | Nasal/oronasal/full-face mask, mouthpiece | Tracheostomy tube |
| Invasiveness | Non-invasive | Surgical airway required |
| Patient comfort | Generally better | Less comfortable |
| Risk of infection | Low (e.g., skin breakdown, conjunctivitis) | High (e.g., ventilator-associated pneumonia, tracheitis) |
| Monitoring needs | Moderate (e.g., adherence, basic vitals) | Intensive (e.g., continuous capnography, frequent suctioning) |
| Caregiver demand | Moderate | High (often requires 24/7 skilled support) |
| Training requirements | Basic respiratory care and device operation | Advanced care for tracheostomy, ventilator, and emergency scenarios |
| Portability | Highly portable | Portable with more extensive equipment needed |
| Use in Pediatrics | Yes | Yes (with significantly increased resources and supervision) |
| Common Indications | COPD, OHS, ALS (non-bulbar onset), SMA, restrictive thoracic diseases | Bulbar ALS, central hypoventilation, severe tracheomalacia, failed NIV |
| Mode | Full Name | Clinical Use Case | Advantages |
| CPAP | Continuous Positive Airway Pressure | Obstructive Sleep Apnea (OSA), mild Obesity Hypoventilation Syndrome (OHS) | Simple, effective for upper airway support and maintaining patency |
| BiPAP | Bilevel Positive Airway Pressure | Chronic Obstructive Pulmonary Disease (COPD), OHS, Neuromuscular Diseases (NMDs) with hypoventilation | Supports both inspiration (IPAP) and expiration (EPAP) |
| AVAPS/VAPS | (Average) Volume-Assured Pressure Support | Progressive NMDs (e.g., Amyotrophic Lateral Sclerosis [ALS], Duchenne Muscular Dystrophy [DMD]) | Guarantees a target tidal volume, improves patient-ventilator synchrony |
| S/T Mode | Spontaneous/Timed Mode | Patients with irregular or absent respiratory drive (e.g., Congenital Central Hypoventilation Syndrome [CCHS]) | Provides a backup respiratory rate in case of apnea or insufficient spontaneous effort |
| iVAPS | Intelligent Volume-Assured Pressure Support | Progressive or variable conditions with fluctuating ventilatory needs | Automatically adapts pressure support to maintain ventilation targets based on real-time feedback |
| Condition | Preferred Modality | Comments |
| COPD with chronic hypercapnia | NIV (BiPAP, iVAPS) | Proven to reduce mortality and hospitalizations (e.g., ERS guidelines) |
| Obesity Hypoventilation Syndrome (OHS) | NIV (CPAP/BiPAP) | CPAP for OSA-predominant OHS; BiPAP for those with significant daytime hypercapnia |
| ALS (non-bulbar onset) | NIV (BiPAP, AVAPS) | NIV as first-line; mouthpiece ventilation is an option for daytime support |
| ALS (bulbar involvement) | IMV | Requires tracheostomy due to high aspiration risk and inability to manage secretions |
| Congenital Central Hypoventilation Syndrome (CCHS) | IMV | Usually requires 24/7 ventilatory support with tracheostomy from early life |
| Pediatric NMD (e.g., SMA, DMD) | NIV → IMV (as needed) | Often starts with NIV; progression to IMV based on bulbar function deterioration or respiratory failure |
| Feature | Description |
| Ventilation modes | Multiple advanced modes (CPAP, BiPAP, AVAPS, pressure/volume control, S/T, iVAPS) |
| Portability | Lightweight, compact, battery-operated for 6–12+ hours of independent use |
| Safety alarms | Integrated alerts for leak detection, apnea, disconnection, and power failure |
| Data monitoring | On-device storage and seamless wireless/cloud-based uploads for therapy review |
| Telemonitoring support | Remote setting adjustment by clinicians and real-time patient compliance tracking |
| Compatibility | Works seamlessly with oxygen concentrators, humidifiers, and various tracheostomy circuits |
| User interface | Intuitive color screen, touch display, and programmable day/night modes for ease of use |
| Examples | Philips Trilogy Evo, ResMed Astral, Breas Vivo 50, LTV 1200 |
Clinical Indications & Patient Populations
Home mechanical ventilation (HMV) is now a cornerstone of chronic respiratory failure (CRF) management across diverse clinical populations. This includes individuals with neuromuscular disorders (NMDs), chronic obstructive pulmonary disease (COPD), obesity hypoventilation syndrome (OHS), central hypoventilation syndromes, and severe restrictive thoracic deformities. Increasingly, pediatric populations are also included, particularly children with congenital conditions or progressive respiratory muscle weakness.
Appropriate patient selection is essential to avoid complications and optimize benefits. According to Park and Suh (2020), successful HMV implementation requires physiological evidence of chronic hypoventilation (e.g., daytime PaCO₂ > 45 mmHg), poor sleep quality, declining pulmonary function (e.g., forced vital capacity [FVC] < 50%), or frequent respiratory exacerbations (13). Studies from Canada, Europe, and Asia consistently confirm that timely HMV initiation improves survival, increases hospital-free days, and enhances the quality of life in eligible patients (14, 15).
Chronic Obstructive Pulmonary Disease (COPD)
Home mechanical ventilation (HMV) has become standard in managing severe Chronic Obstructive Pulmonary Disease (COPD), particularly for patients with persistent hypercapnia (PaCO₂ > 52 mmHg), especially following acute exacerbations.
The landmark HOT-HMV trial and subsequent reviews confirmed significant reductions in mortality and rehospitalization rates when high-intensity non-invasive ventilation (NIV) is applied post-discharge (16, 17). Modes like Average Volume-Assured Pressure Support (AVAPS) and BiPAP-Spontaneous/Timed (BiPAP-ST) are often utilized to improve ventilation efficiency and optimize nocturnal gas exchange in this population.
Key findings regarding HMV in COPD:
- High-intensity NIV demonstrably improves survival in severe COPD.
- AVAPS specifically adapts to ventilatory demand and has been shown to reduce CO₂ more effectively than conventional pressure support modes.
The best candidates for HMV in COPD are typically hypercapnic patients recovering from an acute exacerbation.
Obesity Hypoventilation Syndrome (OHS)
Obesity Hypoventilation Syndrome (OHS), characterized by a Body Mass Index (BMI) over 30 kg/m² and a partial pressure of carbon dioxide (PaCO₂) exceeding 45 mmHg, is frequently accompanied by obstructive sleep apnea (OSA). Research indicates that Bilevel Positive Airway Pressure (BiPAP) or Average Volume-Assured Pressure Support (AVAPS) provides superior carbon dioxide (CO₂) control and reduces daytime somnolence. Continuous Positive Airway Pressure (CPAP) remains a viable option for milder OHS cases, particularly when OSA is the predominant issue. Duiverman (2021) highlighted the critical role of early diagnosis and remote monitoring in ensuring long-term patient adherence to therapy (18).
Clinical Highlights:
- CPAP is the first-line treatment for OHS that’s predominantly driven by Obstructive Sleep Apnea (OSA).
- NIV (BiPAP/AVAPS) is necessary for patients with persistent hypercapnia or those experiencing ventilatory decompensation.
- Monitoring adherence is crucial for the long-term success of HMV in OHS patients.
Neuromuscular Diseases (NMDs)
HMV is life-prolonging in progressive NMDs like ALS, SMA, Duchenne Muscular Dystrophy (DMD), and Myotonic Dystrophy. NIV (BiPAP or AVAPS) is started when FVC falls below 50%, or nocturnal hypoventilation symptoms emerge. For advanced ALS with bulbar dysfunction, tracheostomy with IMV is indicated (7).
Innovative strategies such as mouthpiece ventilation (MPV) promote daytime independence without impeding speech or eating. Chowdhury et al. (2024) reported that MPV improves quality of life in high-functioning ALS patients (11).
Central Hypoventilation Syndromes
These include congenital central hypoventilation syndrome (CCHS) and acquired forms due to brainstem injury or tumors. IMV through tracheostomy is the standard in infants and young children. However, NIV may be used in older children as respiratory control improves (3, 15).
Key considerations:
- Requires long-term ventilation, often 24/7.
- Advanced monitoring (capnography, telemetry) is crucial for safety.
- Transition planning needed in adolescence.
Restrictive Chest Wall Disorders
Patients with kyphoscoliosis, post-polio syndrome, or thoracoplasty experience reduced chest wall compliance, leading to nocturnal hypoventilation. BiPAP and volume-assured pressure modes improve sleep quality, gas exchange, and reduce nocturnal desaturation.
Pediatric Indications
Pediatric use of HMV is expanding, particularly for children with bronchopulmonary dysplasia (BPD), tracheobronchomalacia, and neuromuscular or metabolic disorders. Siddaiah et al. (2025) and Czajkowska-Malinowska et al. (2022) observed marked improvement in survival and caregiver satisfaction in home-ventilated children (4, 19). Pediatric patients often require 24-hour IMV, humidification, suctioning, and complex emergency support protocols.
| Disease | Ventilation Type | Preferred Mode | Clinical Notes |
| COPD (severe hypercapnic) | NIV | BiPAP, AVAPS | Start post-exacerbation |
| Obesity Hypoventilation Syndrome | NIV | CPAP → BiPAP/AVAPS | CPAP in OSA; BiPAP for hypercapnia |
| ALS (non-bulbar) | NIV → MPV | BiPAP, MPV | Tracheostomy in bulbar onset |
| ALS (bulbar involvement) | IMV | Volume or pressure control | Requires intensive care |
| CCHS | IMV → NIV (age-based) | S/T or pressure modes | 24-hour support often required |
| Kyphoscoliosis | NIV | BiPAP, iVAPS | Improves sleep and gas exchange |
| Pediatric BPD/tracheomalacia | IMV | Pressure control | Home-based PICU setup needed |
Referances
- Fagondes, S. C., da Silva, C. L. O., Hoffmann, A., & colleagues. (2025). Home mechanical ventilation: A narrative review and a proposal of practical approach. Brazilian Journal of Pulmonology. https://doi.org/10.1016/j.jornaldepneumologia.2024.11.003
- Scheller, L. L. (2025). Neighborhood-level disparities and health outcomes among children on long-term mechanical ventilation via tracheostomy. eScholarship, University of California. https://escholarship.org/uc/item/75p0v02n
- Perez, G. F. (2024). Management strategies for long-term pediatric mechanical ventilation. In Prolonged and Long-Term Mechanical Ventilation in Pediatrics (pp. 47–64). Springer. https://doi.org/10.1007/978-981-97-8903-0_3
- Siddaiah, R., McKinney, R. L., House, M. A., & colleagues. (2025). Outcomes of ventilator‐dependent children with severe bronchopulmonary dysplasia and tracheobronchomalacia. Pediatric Pulmonology. https://doi.org/10.1002/ppul.71100
- Ong, W. H., Ireland, P., Ho, C. K., & colleagues. (2025). Transcutaneous CO₂ measurement in an adult long-term ventilation (LTV) service. Journal of Clinical Medicine, 14(12), 4137. https://doi.org/10.3390/jcm14124137
- Morrison, S., Gavey, R., Moman, A., Kwiatkowski, S., Duce, B., Hukins, C., & Ellender, C. (2024). P066 Long-term outcomes from home invasive mechanical ventilation in Queensland. Sleep Advances: A Journal of the Sleep Research Society, 5(Suppl 1), A51–A52. https://doi.org/10.1093/sleepadvances/zpae070.148
- Toussaint, M., Wijkstra, P. J., McKim, D., Benditt, J., Winck, J. C., Nasiłowski, J., & Borel, J. C. (2022). Building a home ventilation programme: population, equipment, delivery and cost. Thorax, 77(11), 1140–1148. Advance online publication. https://doi.org/10.1136/thoraxjnl-2021-218410
- Yalwar, A., & Sarkar, G. C. (2025). Cost-effective Bluetooth technology-based emergency medical ventilator for respiratory support: A review. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.5289358
- Wei, Y. J., Dai, S. J., Chen, Y. J., & Lin, Y. J. (2025). Development and use of home ventilators for pediatric care. Pediatric Respirology and Critical Medicine. https://journals.lww.com/prcm/_layouts/15/oaks.journals/downloadpdf.aspx?an=02088913-202504000-00003
- Enzer, K. G., Dawson, J. A., Langevin, J. A., & colleagues. (2025). Medical and social factors associated with prolonged length of stay for chronically ventilated children. Pediatric Pulmonology. https://doi.org/10.1002/ppul.27320
- Chowdhury, A. M., Draicchio, D., & Goodin, C. (2024). Patient-reported outcomes of mouthpiece ventilation in neuromuscular conditions. Thorax, 79(Suppl 2), A55.2. https://thorax.bmj.com/content/thoraxjnl/79/Suppl_2/A55.2.full.pdf
- Louie, K., Amatya, S., Alpan, G., & Parton, L. A. (2024). Non-invasive ventilation with neurally adjusted ventilatory assist (NAVA) improves extubation outcomes in extremely low-birth-weight infants. Children, 11(10), 1184. https://doi.org/10.3390/children11101184
- Park, S., & Suh, E. S. (2020). Home mechanical ventilation: back to basics. Acute and critical care, 35(3), 131–141. https://doi.org/10.4266/acc.2020.00514
- MacIntyre, E. J., Asadi, L., & McKim, D. A. (2016). Clinical outcomes associated with home mechanical ventilation. Canadian Respiratory Journal, 2016, 6547180. https://doi.org/10.1155/2016/6547180
- Kotanen, P. (2023). Home mechanical ventilation and long-term oxygen treatment – prevalence and survival. Helsingin yliopisto. https://helda.helsinki.fi/bitstream/handle/10138/355572/Kotanen_Petra_dissertation_2023.pdf?sequence=1&isAllowed=y
- Murphy, P. B., Rehal, S., Arbane, G., Bourke, S., Calverley, P. M. A., Crook, A. M., Dowson, L., Duffy, N., Gibson, G. J., Hughes, P. D., Hurst, J. R., Lewis, K. E., Mukherjee, R., Nickol, A., Oscroft, N., Patout, M., Pepperell, J., Smith, I., Stradling, J. R., Wedzicha, J. A., … Hart, N. (2017). Effect of Home Noninvasive Ventilation With Oxygen Therapy vs Oxygen Therapy Alone on Hospital Readmission or Death After an Acute COPD Exacerbation: A Randomized Clinical Trial. JAMA, 317(21), 2177–2186. https://doi.org/10.1001/jama.2017.4451
- Jen, R., Ellis, C., Kaminska, M., et al. (2023). Noninvasive HMV for stable hypercapnic COPD: Canadian Review. Canadian Respiratory Journal, 2023, 8691539. https://doi.org/10.1155/2023/8691539
- Duiverman, M. L. (2021). Home mechanical ventilation: setup and monitoring protocols. Pulmonology, 27(1), 1–9. https://doi.org/10.1016/j.pulmoe.2020.08.002
- Czajkowska-Malinowska, M., Bartolik, K., et al. (2022). Development of home mechanical ventilation in Poland: 2009–2019. Journal of Clinical Medicine, 11(8), 2098. https://doi.org/10.3390/jcm11082098